Contributor Dr. Elise Herman
Measles cases are on the rise, and although numbers in the US are small right now, there is cause for concern. Measles is one the most contagious human viruses, with a 90% chance of someone who is not immune getting infected if they are near someone with measles. People with measles can infect others for 4 days before they have any signs of being sick, and for 4 days after the rash appears. The virus stays in the air and is infectious for 2 hours after the infected person has left. There is no treatment for the measles virus, however there is life-long immunity (protection) after vaccination as well as infection.
This recent rise in measles in the US is in part due to a mild drop in kids’ vaccination rates, often related to children missing routine health care visits during the pandemic. Although the current rate of kindergarteners fully vaccinated against measles is good at 92%, the previous rate of 95% was better particularly because that level gives ‘herd immunity’, meaning protection of those that were not or could not be vaccinated (due to young age, cancer treatment, or other immune system problems) by those who are vaccinated.
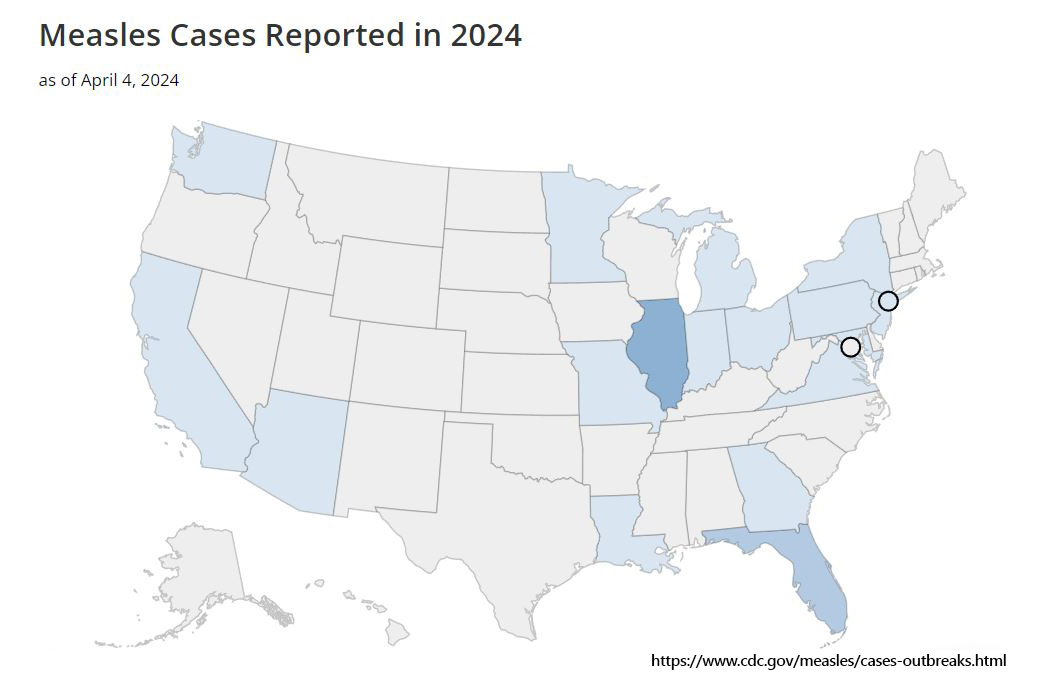
The number of measles infections world-wide has increased dramatically, up almost 80% in the last year to 306,000 cases. As people travel more, they can bring the infection home if they are not immune, potentially exposing many people before they know they are sick.
Measles spreads easily through airborne secretions from coughing or sneezing. Infection is also caused by direct contact with droplets from the mouth, nose, or throat. Symptoms develop 7-14 days later and start with profuse runny nose, cough, and red, swollen, watery eyes. Fever is often up to 104 degrees. The rash develops 3-5 days after cold symptoms begin and starts as flat red spots on the forehead, spreading downwards to the trunk and extremities. Some spots may become raised and join to from larger blotches. It is not usually itchy.
Measles itself is miserable, but the biggest concern is regarding complications. Serious complications include pneumonia in 1 out of 20 of those infected, encephalitis (brain inflammation and swelling) in 1 out of 1000 infected, and rarely, temporary or permanent blindness (more common in developing countries). One out of 5 unvaccinated people in the US with measles will be hospitalized, and 1-3 out of 1000 will die. Children under 5 and adults over 20 are most at risk of serious complications. Also at increased risk are pregnant women and those with immune system problems.
Measles vaccination is safe and effective and gives life-long immunity. Prior concern of a connection between the MMR (measles, mumps, and rubella) vaccine and possible autism was based on fake ‘research’ and has been disproven by multiple studies by the American Academy of Pediatrics, the World Health Organization, and the Institute of Medicine.
There has been a 99% decrease in measles cases since the vaccine came out in 1963. Prior to the vaccine, there were 3-4 million cases annually in the US and about 48,000 people hospitalized, most of which were children. Add approximately 500 deaths and 1,000 cases of encephalitis each year, and it is easy to see how miraculous vaccination has been.
The best way to protect ourselves, as well as the approximately 9 million people in the US who cannot get the vaccine due to an immune system problem, is to be vaccinated. Measles vaccine is recommended for kids aged 12 months and again between 4 and 6 years. It is also approved for adults who did not receive it as children. There are 2 types of measles vaccines- the MMR (as above) and the MMRV (also protects against varicella/chickenpox). Your child’s health care provider can provide additional information on measles vaccination.
more about The contributor

Dr. Elise Herman
Dr. Herman is passionate about community health outreach, school programs, and child/family health and wellness. She has more than 31 years of experience as a pediatrician in Ellensburg, Washington, the last 3 with KVH Pediatrics. In 2022 Dr. Herman mostly retired from practice and continues to contribute blog posts and remain a visible advocate for kids in the community.