After forty six years as a nurse, KVH Chief Nursing Officer Vicky Machorro has decided that come Spring 2023, it’s time to stop setting an alarm clock…
KVH Stories
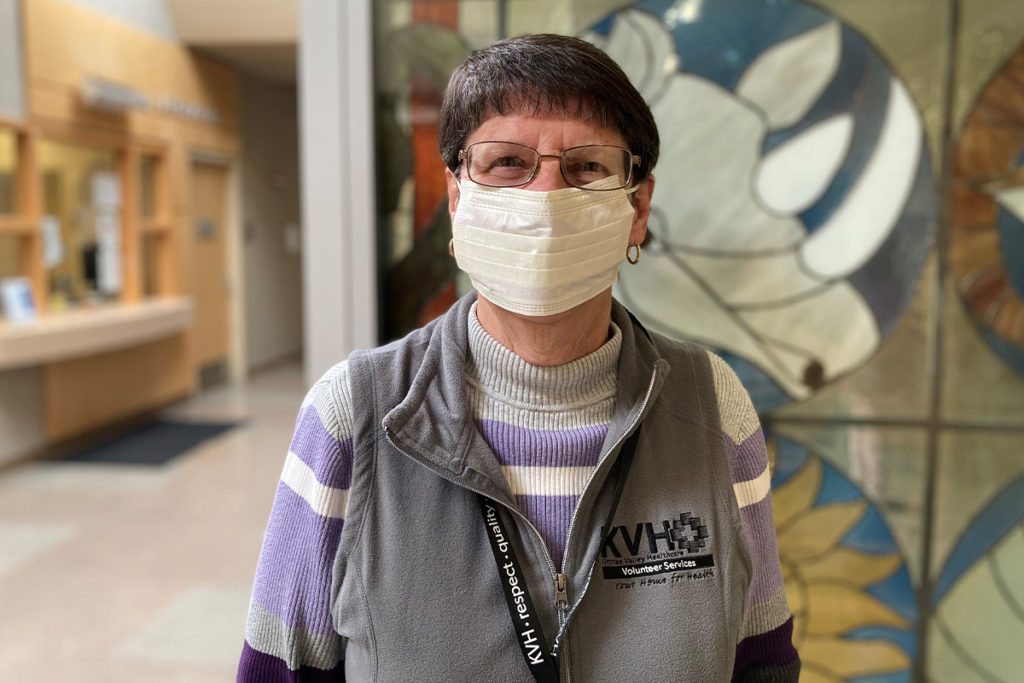
Mary Holmgren (KVH Volunteer)
In 2022, April 17-23 is National Volunteer Week. It was early 2002 when Doug and Mary Holmgren, freshly retired, moved east to be near to their children’s growing families. Not […]
Tony Nelson (COVID-19)
Reliable friend. Life of the party. Hardworking. People person. That’s how Anthony Nelson’s friends and family have always described him. With a quick wit, sharp intellect and enviable social skills, […]
Debbie Hulbert (Inpatient Care)
Debbie Hulbert loved to work in her garden, growing vegetables. A graphic designer by trade, she also loved to cook and paint, and had plenty of energy to do it […]
Betty Osborne (Neurology)
KVH has welcomed a new Neurologist to our specialty team. His name is Dr. Andrew R. Gustavson. Dr. Gustavson comes to KVH with expert training in both Neurology and Psychiatry.
Colton Harlin (Emergency Surgery)
At the tender age of 10, Colton Harlin was generally used to the bruises and scrapes of pee wee football. And when the goal is a quarterback sack, a little […]
David Martin (H1N1)
Prior to coming to the US, the flu season began this year in Australia. US drug companies learned the vaccine they had prepared for the 2019/20 season was not very […]
David Martin (H1N1)
David Martin hadn’t felt well for several days. “You don’t go running to the doctor for the first little sniffle,” admits his wife, Jennifer. Still, she suggested he get checked out, just in case.
Nigel McNeill (General Surgery)
He’s a 38-year-old father of four with an active lifestyle, a passion for volunteerism, and a job he loves as a firefighter/EMT for Grant County Fire District No. 3 in Quincy.